If you’ve ever struggled with PCOS symptoms, you’ll no doubt have already wondered how best to eat to support your PCOS diagnosis. This is such a common question in my clinic and if you have PCOS, you are likely to have spent time on Dr Google trying to find the answer. You’ll have probably found a bunch of conflicting advice that often means giving up foods you love and overly restrictive diets that are too hard to maintain.
So, here is a no-nonsense guide to some simple changes you can make to the way you eat to support your PCOS without rules or restrictions.
Quick reminder- what is PCOS?
Polycystic ovary syndrome or PCOS is an endocrine disorder, meaning it impacts your hormones and is thought to affect at least 5-10% of women. Although recent studies suggest this could be much higher, and it is estimated that it impacts approximately 116 million women worldwide. It can be a complex condition that can be difficult to understand and often there is little support offered to those who receive a diagnosis; leading to feelings of anxiety, confusion and self-blame.
PCOS is characterised by higher androgen levels (e.g. testosterone), menstrual irregularities (missed, irregular or painful periods) and polycystic ovaries (fluid filled sacs surrounding the ovaries). If you have two or more of these features, then you can be diagnosed with PCOS.
Symptoms can range from mild to severe and common symptoms include:
- Irregular or absent periods
- Reduced fertility
- Dark or thick facial and or body hair (Hirstuism)
- Acne or oily skin
- Hair loss from the scalp (alopecia)
- Having higher body weight or difficulty losing weight
- Depression and Anxiety
- Fatigue
How can I eat to improve and support my PCOS symptoms?
Understandably, women want to deal with their symptoms as best as they can, to reduce the negative impacts of these on their quality of life. The good news is that there are some simple strategies that you can implement to do just this.
Of course, diet alone cannot completely remove all symptoms or cure PCOS, but some of these simple strategies may make your symptoms feel more manageable.
Insulin resistance and PCOS
Insulin is a hormone and is the key to open your cells to allow glucose (energy) in. Those with PCOS are more likely to develop insulin resistance. This means that the cells are less responsive to insulin, which can cause higher circulating levels of insulin and sugars in the blood.
Insulin resistance can lead to several problems if left untreated, such as development of type-2 diabetes and inflammation. Insulin can also increase appetite, and women with PCOS and insulin resistance often report feeling hungrier more quickly after meals and having intense cravings for foods. This can be for a number of reasons but taking steps to help manage blood sugars can be a helpful way to reduce this issue.
Eat regularly
If you have PCOS, eating regularly is important. Aiming to eat every 3-5 hours through three meals a day and snacks if needed, will help to keep blood sugars more stable which can help with insulin resistance and appetite.
Plate Planning
Plate planning allows you to think about what to add to your plate without having to measure or count anything.
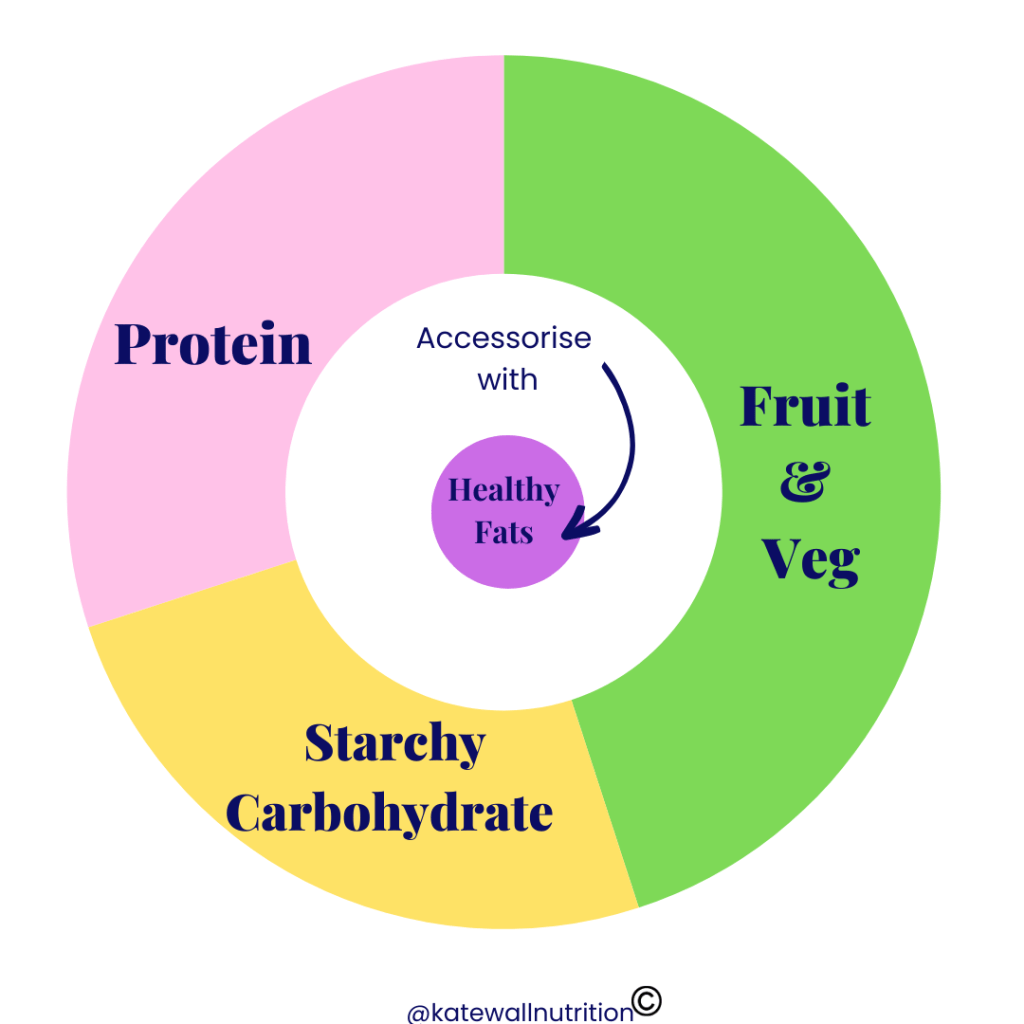
If most of your meals contain protein, starchy carbohydrates, fruits and veg (more veg than fruit) and some healthy fats then you are eating balanced meals.
In terms of how much of each of these to eat; the standard advice is to think about dividing your plate into thirds (veg, protein and carbohydrates) and then ‘accessorise’ with healthy fats.
In those with PCOS, I would generally advise increasing the veg and protein section a little more and reducing the carbohydrates a little, as a slightly higher protein and fibre diet has been seen to be beneficial to androgen levels and insulin resistance in PCOS.
The picture below is a visual to bring to mind to help you when putting a meal together- obviously, this is not exact proportions but offers a rough guide to how to put a plate of food together to support PCOS. Remember, you don’t need to get every meal ‘perfectly’ balanced in this way, but if most of your meals use this plate planning approach then you will be a long way towards eating well for PCOS.
By combining carbohydrates with proteins, fibre and fats, this will slow down digestion and give a more gradual rise to your blood sugars, along with giving the best combination to feel fuller for longer and satisfied after your meal, meaning less cravings and hunger pangs.
Low GI
All foods have a glyceamic index, which in simple terms is the speed at which a food raises your blood glucose level. Each time you eat, your blood sugar will rise, but some foods are digested more quickly than others causing a sharper rise – these are classed as high GI foods. Ingredients that are digested more slowly are classed as low GI foods and the blood sugar levels will rise more slowly after eating these.
It is important to note that high GI foods are not ‘bad’ foods, in fact sometimes healthier options have a higher GI. For example, some crisps may have a lower GI than baked potato because of the fat content but the potato is a healthier choice. However, lower GI carbohydrates will impact on blood sugar levels less, and by including these foods it has been shown to benefit those with PCOS by reducing insulin resistance, androgen levels and improving menstrual regularity.
Here are some everyday examples of lower GI carb choices that can help you to support your body in PCOS:
- Wholegrain, granary, rye, seeded bread, sourdough bread
- New potatoes in their skins, sweet potato, yam, cold boiled potatoes
- Wholegrain pasta cooked until al dente, noodles
- Basmati rice, long grain or brown rice
- Bulgur wheat, barley, couscous, quinoa
- Porridge, muesli, some low-sugar oat and bran-based cereals
Mediterranean style Diet
The Mediterranean style diet is one of the most researched dietary patterns and has been shown to have health benefits in many areas, including PCOS.
Some of the benefits include:
- Reduced inflammation
- Reduced androgens and insulin resistance
- Improved mental health
- Increased gut microbiota diversity (which can often be lower in PCOS and is thought to be linked to some symptoms).
Omega-3
Omega-3’s are essential fatty acids (we can only get them from foods) and are really important to everyone’s health, but they have specific value to those with PCOS as they can help to reduce inflammation, which is a driving force of many PCOS symptoms. Omega-3’s have also been found to improve lipid profiles (cholesterol and triglycerides), which is important as PCOS can have an increased risk of heart disease and so eating to support heart health is important.
The best source of omega-3’s is oily fish such as mackerel, salmon or sardines. Aim for 1-2 portions of 140g a week. Plant based foods such as chia seeds, flaxseeds and walnuts contain a plant-based version of omega three. However they’re not used efficiently by the body, so will not provide a rich Omega-3 source. They should supplement the oily fish.
Summary
Simple changes such as regular eating and balanced meals can be a great start to improving your symptoms through your dietary pattern. Of course, areas such as sleep, stress management and movement are all going to be important too but making sure you are nourishing your body to give you the energy and brain power to do those other things is a great start. There is a lot of misinformation on diet and PCOS out there, so do watch out and bottom line – keep it simple!
PCOS is a complex condition and may require medical, psychological and nutritional support to be able to adequately manage the symptoms. Many women living with PCOS face difficulties such as body image issues or disordered eating and making dietary changes and therefore challenging. If you need support with this, or if you’re still unsure how best to eat to support your PCOS then you can always reach out for help.




